April 9, 2020
Richard Pilch
This article is part of World War “V”: The COVID-19 Pandemic, a collection of all CNS COVID-19-related articles.
On April 7, 2020, the Wall Street Journal reported that the Federal Emergency Management Agency (FEMA) has been unable to secure critical supplies from industry to support the US COVID-19 response.[1] But many of the needed items do exist in hospitals and medical clinics across the country. In this article, we propose an approach to leverage supply surplus, as well as other sharable assets, between stable areas of the country and areas in need. Our approach is grounded in both US and international practice, including the US All-Hazards National Mutual Aid System.[2] For unclear reasons, FEMA’s four-pronged approach to sourcing medical supplies[3] does not mention this existing mutual aid system, which is state law in all 50 states and the District of Columbia. Importantly, any such pairing strategy would require regional controls to protect stable areas from imported COVID-19 cases as assets are surged to areas in need.

Touro Infirmary in Uptown New Orleans added walk-in testing for Coronavirus on 2020-03-21 (Src: Paulscrawl, Wikimedia Commons)
One often-overlooked cornerstone of China’s COVID-19 response was a pairing strategy that assigned each affected city in Hubei province, where the outbreak was ongoing, with a province of China responsible for providing the affected city with medical aid spanning personnel, equipment (e.g., mechanical ventilators), and supplies (e.g., masks, gloves).
China’s strategy recognized one of the key risks to Hubei—that the exponential rise in cases would rapidly overwhelm local healthcare systems. But the strategy was forced to balance this reality against a competing risk that the rapid spread of COVID-19 to these contributing provinces would leave them less protected after providing aid to Hubei. In the end, the strategy appears to have paid off, at least in the short term—the influx of medical personnel, equipment, and supplies helped stem the tide of the outbreak in Hubei, while outside provinces remained comparatively stable.
The United States now finds itself in a similar situation to China in January: the exponential rise in cases has already threatened healthcare capacity in New York City with other cities expected to soon follow, while other parts of the country remain relatively spared—at least for now. These spared areas are making preparations for impending cases as best they can, which is critical to protecting their populations. But by redirecting a subset of their personnel, equipment, and supplies to areas in need, spared areas may contribute far more to both the national response and their own long-term outlook, enabling the US to better contain COVID-19 hotspots while accelerating the timeline to economic recovery.
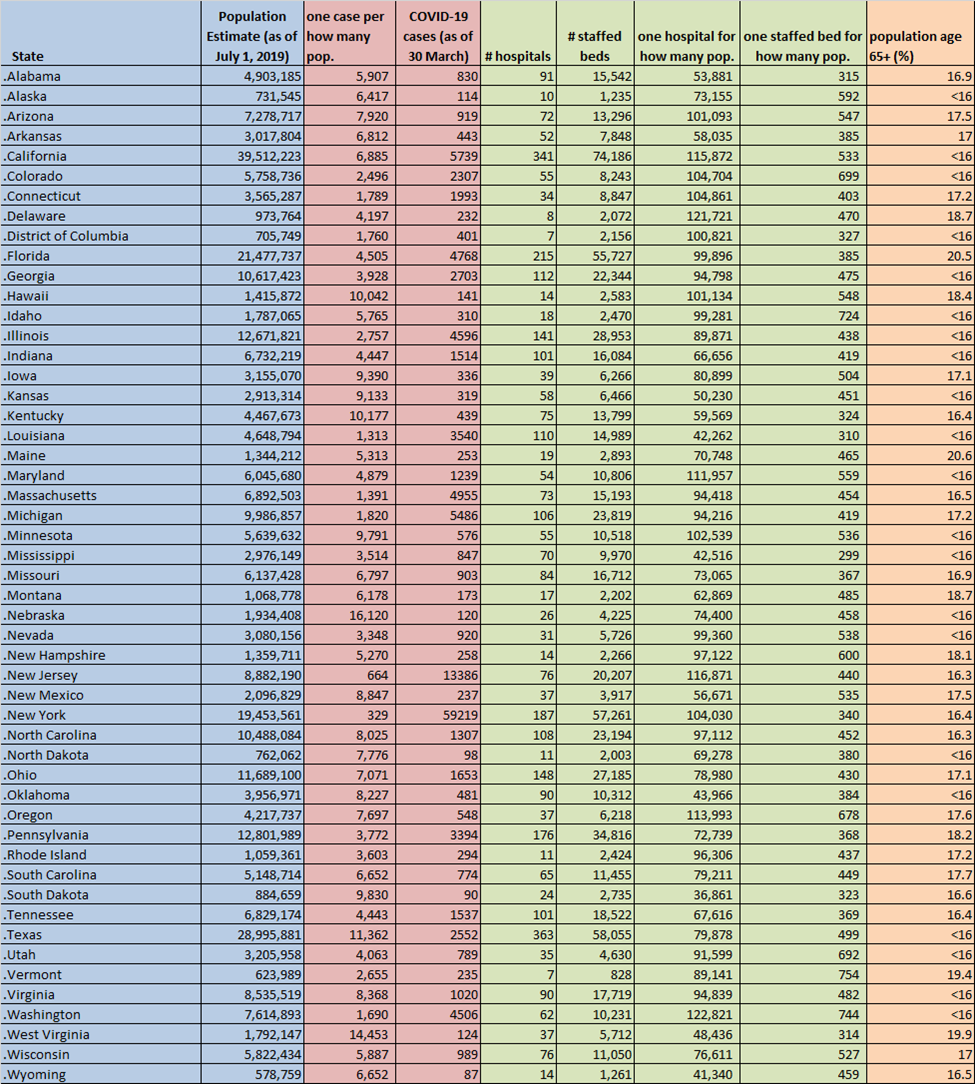
We compared state COVID-19 case load as a function of each state’s population to identify immediate and imminent areas of need. We then conducted a preliminary analysis of each state’s healthcare capacity using two metrics, hospitals and staffed beds per population, to gain a general understanding of which states may have a general healthcare surplus. Finally, we considered each state’s proportion of residents over 65 years of age to gain some understanding of which states are at higher risk of critical infections based on population age.
Our analysis identified 11 priority areas in immediate need, defined as areas with one or more COVID-19 cases per 3,000 population. We grouped New England states for simplicity, reducing the number of priority areas to 9. While we recognize that COVID-19 cases per 3,000 population is not an ideal metric, it is consistently quantifiable thus reducing bias in our analysis. For example, using this approach, California’s relatively high total case count of 5,739 as of 30 March 2020 is offset by a state population of more than 39 million; it can therefore be reasonably expected that California will divert resources internally from lower risk areas to higher risk areas in the same way that we are proposing at the national level.
Our analysis further identified 15 stable areas with surplus, defined as areas with less than one COVID-19 case per 6,000 population AND one staffed hospital bed per 500 or less population. We grouped areas of stability and surplus regionally to reduce the total number of areas to 9. Again, we recognize that this is an imperfect metric to demonstrate potential healthcare capacity above current COVID-19 need; it is quantifiable thus reducing bias, but is not necessarily reflective of specific personnel, equipment, and materials of relevance.
We then paired our results to match areas in immediate need with areas of surplus and relative stability, as presented in the following table. The table is presented in rank order by immediate need metric. We considered geographic proximity to the extent feasible during the matching process. The full data set is provided as an Appendix at bottom.
| Priority | Area in Immediate Need | Stable Area with Surplus |
|---|---|---|
| 1 | New York | Upper Central US (Nebraska, North Dakota, South Dakota) |
| 2 | New Jersey | Lower Central US (Texas, Oklahoma, Kansas) |
| 3 | Louisiana | Arkansas |
| 4 | New England (Massachusetts, Connecticut, Vermont) | Carolinas (North Carolina, South Carolina) |
| 5 | Washington | Montana |
| 6 | District of Columbia | Virginias (Virginia, West Virginia) |
| 7 | Michigan | Ohio |
| 8 | Colorado | Wyoming |
| 9 | Illinois | Kentucky |
This analysis is meant to present the concept of regional pairing given limited data and time. We expect that with more robust data, a more precise pairing methodology can be utilized that best tailors matches.
To make such an approach work, a number of key steps must be taken:
- Incentivization to Donor Areas. Stable areas with surplus that agree to contribute personnel, equipment, and/or supplies must be compensated above and beyond the value of their contributions. The value of their contributions includes wage offsets, equipment “rental” payments, and supply reimbursement in kind. Additional compensation may be in the form of interest payments based on contribution value; future partnership, for example commitments by recipient states to purchase specified levels of goods or services from donor states; or offset projects, whereby recipient states fund developmental programs of need in donor states. We recommend this incentivization activity be negotiated at the state level but conducted and coordinated by the federal government, which would maintain oversight and accountability of material shipments, storage, and distribution.
- Protection of Donor Areas. As discussed, by providing personnel, equipment, and/or supplies to areas in need, donor areas become more vulnerable to COVID-19. Thus, these areas must be protected by strict border control, rigorous surveillance and early case identification, and rapid contact tracing and quarantine. We recommend this protection be provided in full by the federal government. In addition, any healthcare workers traveling to areas in need must be carefully screened and quarantined upon return in order to ensure that the virus is not inadvertently introduced; we recommend this action be carried out by each donor state directly.
- Assurances of Asset Replacement/Return, Redistribution, and Mutual Support. We expect the US COVID-19 case load to continue to rise nationally as areas of high population density are affected and subsequently recover from localized outbreaks. This means that there will likely be a lag in case load from city to city, necessitating the continued sharing of assets with populations of greatest need. If donor areas are next affected, then consumed supplies (i.e., “consumables”) must be immediately backfilled by the federal government as other assets are rapidly returned. If non-donor areas are next affected, assets must be redistributed accordingly. This will require a level of vigilance, flexibility, and speed in the face of difficult resource allocation decisions, and should be the responsibility of the federal government.
We recognize the considerable risk to donor areas that this strategy presents. While such calculated risks may be recommended at the national level, states must carefully weigh this strategy against many others designed to limit the impact of COVID-19 on their populations. This author believes that donor state populations would be best protected by sharing resources in order to limit public health and economic impact on the nation, reduce COVID-19 spread, and accelerate recovery. But I also believe an approach such as this must remain voluntary on the part of donor states. The same would be said of a similar strategy among European Union nations.
As we have seen with so many global health challenges preceding COVID-19, some populations are affected while others help—sometimes to preserve their own populations, sometimes simply out of good will. In the end, it is not the motivation that matters but the recognition that we are a united population—where one fails, we all do.
Dr. Richard Pilch is Director of the Chemical and Biological Weapons Nonproliferation Program, James Martin Center for Nonproliferation Studies, Middlebury Institute of International Studies at Monterey.
See Also
 World War “V”: The COVID-19 Pandemic
World War “V”: The COVID-19 Pandemic
A collection of all CNS COVID-19-related articles
NOTES
[1] https://www.wsj.com/articles/at-fema-companies-offer-critical-coronavirus-supplies-the-government-cant-buy-11586276450 [2] https://www.emacweb.org/ [3] https://www.fema.gov/fema-supply-chain-task-force-leads-four [4] See, for example, http://www.xinhuanet.com/english/2020-02/16/c_138789227.htm [5] Note that Alabama met the inclusion criterion for surplus but was just over one COVID-19 case per 6,000 population, and Iowa met the inclusion criterion for current case load but has just less than one staffed bed per 500 population. Thus, neither was included. In addition, New Mexico met the criterion current case load and displayed a high metric for hospitals per population did not meet the staffed beds per population metric and thus was not included. We set a cutoff of 20% over age 65 to remove any high risk populations from analysis.Appendix
Population data – US Census Bureau, https://www.census.gov/data/tables/time-series/demo/popest/2010s-state-total.html
COVID-19 case data – US Centers for Disease Control and Prevention (CDC), https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
State hospital and staffed bed data – American Hospital Directory (AHD), https://www.ahd.com/state_statistics.html
Population age data – Population Reference Bureau, https://www.prb.org/which-us-states-are-the-oldest
See Also
 World War “V”: The COVID-19 Pandemic
World War “V”: The COVID-19 Pandemic
A collection of all CNS COVID-19-related articles