March 6, 2020
Richard Pilch
This article is part of World War “V”: The COVID-19 Pandemic, a collection of all CNS COVID-19-related articles.
Two weeks ago, I was planning a conference in the Milan area focused on global health security threats like COVID-19. On Friday, February 21, there were three COVID-19 cases in Italy, all having traveled from affected areas in China. Today, exactly two weeks later, there are 4,636 cases. That’s how quickly the situation can change with this virus.
Here in California, our medical and public health practitioners are excellent, and they are doing what they are trained to do: identify, isolate, and treat cases of SARS-CoV-2 infection; trace and quarantine close contacts; and promote risk awareness, hand hygiene, and social distancing in the broader population. But what must be recognized is that there is a time delay of days between what we see – confirmed cases of infection – and what is really there: infected individuals who we haven’t yet identified. This delay in identification places us on the same timeline that Milan was two weeks ago. And while it’s true that this combination of rapid transmission plus identification delay is similar to seasonal influenza, there is a major difference: based on our current understanding, COVID-19 is twenty times more lethal than the common flu.
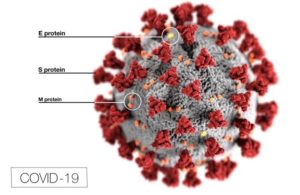
Source: CDC
The Virus is 20x More Lethal Than the Common Flu
Recently, US government officials have begun using the term “community spread” to describe cases of infection not specifically linked to individuals who are known to be infected. They anticipate that we should expect to see—and may already be seeing—more of this “community spread” in the United States. As a medical doctor and public health professional, I find that term misleading. Every case of this virus is connected—transmitted initially from an animal source to humans, and then onward from human to human primarily by respiratory droplets that contain the virus. This respiratory transmission is most efficient from a distance of less than 6 feet; the longer an uninfected person is within 6 feet of someone who is spreading the virus via respiratory droplets, the more opportunity to get infected. This is why we see most cases spreading among family members, and between patients and their healthcare providers.
Where else are individuals within 6 feet of each other for prolonged periods of time? Schools. Churches. Movie theaters. Indoor sporting events. Concerts.
Social Distancing: Six Feet Apart and Advice for Large Events
If we want to get serious about interrupting transmission of this virus, these are the places to start. And the means to do so is to employ rigorous “social distancing” practices in the affected areas of northern California. Accordingly, on March 5, 2020, Santa Clara County—where 24 COVID-19 cases have been identified to date—recommended “postponing or canceling mass gatherings and large community events where large numbers of people are within arm’s length of one another.”
The medical literature supports this approach. A 2018 review article of fifteen studies of influenza transmission found that workplace social distancing reduced overall infection rates, while also buying time for the development of countermeasures such as vaccines. However, the effectiveness of social distancing depended on the speed with which social distancing measures were implemented, along with the compliance of affected individuals.
This isn’t to say that individuals should restrict themselves to their homes indefinitely. But we need to shift our practices, and our messaging, from “remain calm” to “be smart.” Recognize that spending a prolonged period of time in a confined space with a large number of people may be a risk. Because there is no scientific consensus as yet on where to draw the line, consider more than one hour in a confined space with more than 100 people as an arbitrary guideline to pause and consider—will we be face-to-face for extended durations? Will we be interacting with more than just the people near us? Is the ventilation system filtered? Are there alternatives that reduce my risk? And of course if you are sick with fever, cough, shortness of breath, or other flu-like symptoms, do not unnecessarily expose others by going to these places yourself. Finally, recognize that while this article focuses on respiratory transmission, the virus can survive on surfaces for hours to days. Be mindful of what you touch—both around you and on your own body—and wash your hands thoroughly and often.
Today, Austin Texas’ SXSW 2020 was cancelled. Italy has banned fans from its professional soccer games, and France has banned indoor gatherings of more than 5,000 people altogether. Japan has closed schools and resorts. Yet last night, just hours after Santa Clara County issued its recommendation, the San Jose Sharks opened its doors to a home crowd of 14,517.
It was the lowest home attendance of the year—but it’s still too many.
Dr. Richard Pilch is Director of the Chemical and Biological Weapons Nonproliferation Program, James Martin Center for Nonproliferation Studies, Middlebury Institute of International Studies at Monterey.
See Also
 World War “V”: The COVID-19 Pandemic
World War “V”: The COVID-19 Pandemic
A collection of all CNS COVID-19-related articles
