Eric Croddy
October 9, 2001
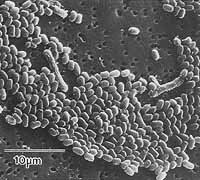
Electron micrograph of Bacillus anthracis spores. Photograph courtesy of USAMRIID
Due to the cases of exposure to Bacillus anthracis and the tragic death of one individual in Florida during the first week of October 2001, there has been an increased amount of attention given to anthrax and the potential bioterrorist threat. This report is only a brief introduction and is not meant to provide any prescriptions, medical or otherwise. [1]
Anthrax Infection Types & Data
Anthrax describes the disease caused by the bacterium Bacillus anthracis, a naturally-occurring organism that has been weaponized in the past by both the United States and former Soviet Union for their respective biological warfare (BW) programs.
There are three major routes of infection for anthrax:
- Cutaneous form — most common
- Gastrointestinal — from ingestion of microorganisms in contaminated meat, for example
- Inhalation
From 1900 to 1978, only 18 cases of inhalation anthrax were reported in the United States, two of these being laboratory acquired infections. The most rare in terms of its natural occurrence, inhalation anthrax is of great interest due to the potential of aerosolized Bacillus anthracis spores for bioterrorism.
Table from US Army Research Institute of Infectious Diseases (USAMRIID) [2]
| Disease | Inhalation anthrax |
|---|---|
| Transmit Man to Man | No |
| Infective Dose (Aerosol) | 8,000-50,000 spores |
| Incubation Period | 1-6 days |
| Duration of Illness | 3-5 days (usually fatal if untreated) |
| Lethality (approx. case fatality rates) | High |
| Persistence of Organism | Very stable-spores remain viable for > 40 years in soil |
| Vaccine Efficacy (aerosol exposure) | 2 dose efficacy against up to 1,000 LD50 in monkeys |
Cutaneous
When faced with lack of nutrients, environmental stress and other factors, Bacillus anthracis can form hardy endospores. These spores can survive for decades in the soil, but also in the hair and other tissues of animal carcasses (e.g., cattle). In rare cases these spores can become aerosolized, often through the processing of animal products used in textiles. Death from inhaling Bacillus anthracis spores, then referred to more commonly as “woolsorter’s disease” or “ragpicker’s disease,” was a frequent hazard during the Industrial Revolution before a vaccine and better ventilation were provided. [3] For veterinarians and other professions at risk of exposure, the more recent development (1950s) of an effective vaccine for anthrax has nearly eliminated cases of inhalation anthrax in North America.
Skin Infection
The skin infection often forms a darkened pustule, thus the name anthrax (from the Greek for coal, e.g., anthracene.) The cutaneous form represents about 95% of all cases worldwide, and is generally treatable. Primarily because the window of opportunity is smaller for detection of the disease, the ingested route of anthrax infection has a poorer prognosis, approximately 50% of such cases are fatal, while the inhalation form is even more deadly. However, treatment with antibiotics of those who have been exposed to anthrax spores (e.g., doxycycline, penicillin, Ciprofloxacin, etc.) is usually successful if caught early enough (before symptoms appear).
Inhalation
Although hemorrhagic meningitis is also seen in other forms of anthrax, it is often expected in the inhalation form. A fuller clinical picture of inhalation anthrax usually presents with a widened mediastinum on the chest x-ray, caused by the hemorrhaging of the regional lymph due to proximity to the site of the inoculation (lungs). Pneumonia is generally not part of the clinical picture. Numbers vary depending upon which model one uses, but generally speaking about 8,000 spores are required to cause infection in humans. If caught early enough following exposure, prophylactic treatment with antibiotics is usually successful. However, anthrax is usually refractory to treatment once the course of infection and symptoms appear.
In 1979, a release of B. anthracis spores from a Soviet biological weapons facility in Sverdlovsk (now renamed Yekaterinberg) killed at least 66 people, but we still do not know the full picture of what happened due to subsequent efforts by Soviet authorities to cover up the disaster. This outbreak may have started with the airborne release of hundreds of grams of bacteria. Although data are still sparse, during the Sverdlovsk incident cases of anthrax emerged anywhere from 2 days to 43 days following exposure. From this and other experimental data, it can be estimated that inhaled anthrax bacterial spores may take up to 60 days before they begin to grow. A complex toxin produced and excreted by Bacillus anthracis (a Gram-positive organism), is actually responsible for the disease process that follows, starting with fever, cough, headache, or a similar constellation of flu-like symptoms lasting hours to a few days. The following stage involves a rapid deterioration, including difficulty in breathing, high fever and shock. At this point, death follows quickly.
Anthrax: Challenging for Bioterrorists
With its “brand-name recognition,” and its relative ease of isolation, growth, and weaponization, anthrax bacteria are at first glance well-suited for bioterrorism. However, the demanding processes involved in the propagation of the bacteria, and the engineering hurdles required for their efficient dissemination would present significant challenges to terrorists attempting to cause mass casualties.
To prepare for the unlikely event of a mass bioterrorist attack on US civilians, the US government has established a National Pharmaceutical Stockpile consisting of over 400 tons of medical supplies, positioned at eight different locations across the United States. These stockpiles contain large quantities of antibiotics, including Ciprofloxacin (the prophylactic of choice for anthrax exposures) and other medicaments to treat victims of a mass casualty attack involving chemical or biological agents.
References
Arthur M. Friedlander, “Anthrax,” in Frederick R. Sidell, Ernest T. Takafuji, and David R. Franz, Textbook of Military Medicine, Part I: Warfare, Weaponry, and the Casualty: Medical Aspects of Chemical and Biological Warfare (Washington, DC:Borden Institute, Walter Reed Army Medical Center, 1997) pp. 467-78.
Terry C. Dixon, Matthew Meselson, Jeanne Guillemin, and Philip C. Hanna, “Anthrax,” (Review article), New England Journal of Medicine, Vol. 341, No. 11, September 9, 1999, pp. 814-26.
David H. Walker, Olga Yampolska, and Lev. M. Grinberg, “Death at Sverdlovsk: What Have We Learned?” American Journal of Pathology, Vol. 144, No. 6, June 1994, pp. 1135-41.
Faina A. Abramova, Lev M. Grinberg, Olga V. Yampolskaya, and David H. Walker, “Pathology of Inhalational Anthrax in 42 Cases from the Sverdlovsk Outbreak of 1979,” Proceedings of the National Academy of Sciences, USA, 1993, pp. 2291-94.
Philip S. Brachman, Arnold F. Kaufmann, and Frederic G. Dalldorf, “Industrial Inhalational Anthrax,” Bacteriological Reviews, Vol. 30, No.3, Sept. 1966, p. p646-57.
Sources:
[1] For more details, the reader is directed to the consensus article by Thomas V. Inglesby, MD; Donald A. Henderson, MD, MPH; John G. Bartlett, MD; Michael S. Ascher, MD; Edward Eitzen, MD, MPH; Arthur M. Friedlander, MD, et al., “Anthrax as a Biological Weapon: Medical and Public Health Management,” in the Journal of the American Medical Association (JAMA), Vol. 281 No. 18, May 12, 1999, pp. 1735-45, http://jama.ama-assn.org.
[2] US Army, Medical Management of Biological Casualties Handbook, Fourth edition (Fort Detrick, MD: USAMRIID, February 2001) pp. 26-35, www.nbc-med.org.
[3] Stanley A. Plotkin; Philip S. Brachman; Milton Utell; Forest H. Bumford and Mary M. Atchison, “An Epidemic of Inhalation Anthrax, the First in the Twentieth Century,” American Journal of Medicine, Vol. 29, No. 6, December 1960, pp. 992-1001.
